Wang Y, Li Z, Zhao X, Wang D, Li H, Xian Y, et al. Stroke care quality in China: Substantial improvement, and a huge challenge and opportunity. Int J Stroke : official journal of the International Stroke Society. 2017;12(3):229–35.
Google Scholar
Ma Q, Li R, Wang L, Yin P, Wang Y, Yan C, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990–2019: an analysis for the global burden of disease study 2019. Lancet Public health. 2021;6(12):e897–906.
Google Scholar
Wang W, Jiang B, Sun H, Ru X, Sun D, Wang L, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–71.
Google Scholar
Wang LDWJ, Peng B, Xu YM. Brief report on stroke prevention and treatment in China, 2019. Chin J Cerebrovasc Dis. 2020;17(5):272–81.
Google Scholar
GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820.
Li Z, Jiang Y, Li H, Xian Y, Wang Y. China’s response to the rising stroke burden. BMJ (Clinical research ed). 2019;364:l879.
Google Scholar
Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405.
Google Scholar
Wang YJ, Li ZX, Gu HQ, Zhai Y, Zhou Q, Jiang Y, et al. China stroke statistics: an update on the 2019 report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. 2022;7(5):415–50.
Google Scholar
Lanctôt KL, Lindsay MP, Smith EE, Sahlas DJ, Foley N, Gubitz G, et al. Canadian stroke best practice recommendations: mood, cognition and fatigue following stroke, 6th edition update 2019. Int J Stroke : official journal of the International Stroke Society. 2020;15(6):668–88.
Google Scholar
Baylan S, Griffiths S, Grant N, Broomfield NM, Evans JJ, Gardani M. Incidence and prevalence of post-stroke insomnia: a systematic review and meta-analysis. Sleep Med Rev. 2020;49:101222.
Google Scholar
Carnes-Vendrell A, Deus J, Molina-Seguin J, Pifarré J, Purroy F. Depression and apathy after transient ischemic attack or minor stroke: prevalence, evolution and predictors. Sci Rep. 2019;9(1):16248.
Google Scholar
Banda KJ, Chu H, Kang XL, Liu D, Pien LC, Jen HJ, et al. Prevalence of dysphagia and risk of pneumonia and mortality in acute stroke patients: a meta-analysis. BMC Geriatr. 2022;22(1):420.
Google Scholar
Harriott AM, Karakaya F, Ayata C. Headache after ischemic stroke: a systematic review and meta-analysis. Neurology. 2020;94(1):e75–86.
Google Scholar
Ali M, Tibble H, Brady MC, Quinn TJ, Sunnerhagen KS, Venketasubramanian N, et al. Prevalence, trajectory, and predictors of poststroke pain: retrospective analysis of pooled clinical trial data set. Stroke. 2023;54(12):3107–16.
Zhang Q, Chen D, Shen Y, Bian M, Wang P, Li J. Incidence and prevalence of poststroke shoulder pain among different regions of the world: a systematic review and meta-analysis. Front Neurol. 2021;12:724281.
Google Scholar
Yang S, Chang MC. Poststroke pain. Semin Neurol. 2021;41(1):67–74.
Google Scholar
Paolucci S, Iosa M, Toni D, Barbanti P, Bovi P, Cavallini A, et al. Prevalence and time course of post-stroke pain: a multicenter prospective hospital-based study. Pain Med (Malden, Mass). 2016;17(5):924–30.
Widar M, Samuelsson L, Karlsson-Tivenius S, Ahlström G. Long-term pain conditions after a stroke. J Rehabil Med. 2002;34(4):165–70.
Google Scholar
Payton H, Soundy A. The experience of post-stroke pain and the impact on quality of life: an integrative review. Behav Sci (Basel, Switzerland). 2020;10(8):128.
Google Scholar
Zhang YH, Wang YC, Hu GW, Ding XQ, Shen XH, Yang H, et al. The Effects of gender, functional condition, and ADL on pressure pain threshold in stroke patients. Front Neurosci. 2021;15:705516.
Google Scholar
Wang K, Liu H. Association between widespread pain and dementia, Alzheimer’s disease and stroke: a cohort study from the Framingham Heart Study. Reg Anesth Pain Med. 2021;46(10):879–85.
Google Scholar
Tang SC, Lee LJ, Jeng JS, Hsieh ST, Chiang MC, Yeh SJ, et al. Pathophysiology of central poststroke pain: motor cortex disinhibition and its clinical and sensory correlates. Stroke. 2019;50(10):2851–7.
Google Scholar
Li C, Shu X, Liu X. Research hotspots and frontiers in post stroke pain: a bibliometric analysis study. Front Mol Neurosci. 2022;15:905679.
Google Scholar
Xiong F, Shen P, Li Z, Huang Z, Liang Y, Chen X, et al. Bibliometric analysis of post-stroke pain research published from 2012 to 2021. J Pain Res. 2023;16:1–20.
Google Scholar
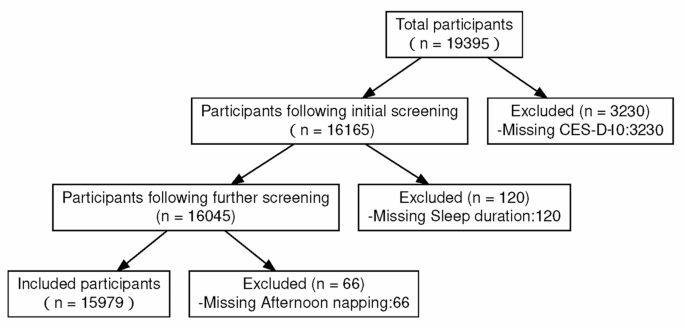
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Google Scholar
Chen H. Mui ACJIP. Factorial validity of the center for epidemiologic studies depression scale short form in older population in China. 2014;26(1):1–9.
Administration NHS. Statistical bulletin on healthcare security 2018. 2019.
Qiu Y, Li H, Yang Z, Liu Q, Wang K, Li R, et al. The prevalence and economic burden of pain on middle-aged and elderly Chinese people: results from the China health and retirement longitudinal study. BMC Health Serv Res. 2020;20(1):600.
Google Scholar
Husky MM, Ferdous Farin F, Compagnone P, Fermanian C, Kovess-Masfety V. Chronic back pain and its association with quality of life in a large French population survey. Health Qual Life Outcomes. 2018;16(1):195.
Google Scholar
Yang L, Peng W. Prevalence and factors associated with body pain: results of a nationally representative survey of 9,586 Chinese adults aged 60 and over. Front Public Health. 2021;9:634123.
Google Scholar
Yu T, Ma J, Jiang Y, Li J, Gen Y, Wen Y, et al. Assessing pain among Chinese Elderly-Chinese health and retirement longitudinal study. Iran J Public Health. 2018;47(4):553–60.
Google Scholar
Klit H, Finnerup NB, Overvad K, Andersen G, Jensen TS. Pain following stroke: a population-based follow-up study. PLoS ONE. 2011;6(11):e27607.
Google Scholar
Hansen AP, Marcussen NS, Klit H, Kasch H, Jensen TS, Finnerup NB. Development of persistent headache following stroke: a 3-year follow-up. Cephalalgia : an international journal of headache. 2015;35(5):399–409.
Google Scholar
Montgomery W, Vietri J, Shi J, Ogawa K, Kariyasu S, Alev L, et al. The relationship between pain severity and patient-reported outcomes among patients with chronic low back pain in Japan. J Pain Res. 2016;9:337–44.
Google Scholar
Tsuji T, Matsudaira K, Sato H, Vietri J. The impact of depression among chronic low back pain patients in Japan. BMC Musculoskelet Disord. 2016;17(1):447.
Google Scholar
Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009;8(8):741–54.
Google Scholar
Atalan P, Bērziņa G, Sunnerhagen KS. Influence of mobility restrictions on post-stroke pain. Brain Behav. 2021;11(5):e02092.
Google Scholar
Tse MM, Tang SK, Wan VT, Vong SK. The effectiveness of physical exercise training in pain, mobility, and psychological well-being of older persons living in nursing homes. Pain Manag Nurs : official journal of the American Society of Pain Management Nurses. 2014;15(4):778–88.
Google Scholar
Ma Y, Luo J, Wang XQ. The effect and mechanism of exercise for post-stroke pain. Front Mol Neurosci. 2022;15:1074205.
Google Scholar
Zhang W, Liu Y, Yu J, Zhang Q, Wang X, Zhang Y, et al. Exercise interventions for post-stroke depression: a protocol for systematic review and meta-analysis. Medicine. 2021;100(8):e24945.
Google Scholar
de Luca KE, Parkinson L, Haldeman S, Byles JE, Blyth F. The relationship between spinal pain and comorbidity: a cross-sectional analysis of 579 community-dwelling, older Australian women. J Manipulative Physiol Ther. 2017;40(7):459–66.
Google Scholar
Lee MK, Oh J. The relationship between sleep quality, neck pain, shoulder pain and disability, physical activity, and health perception among middle-aged women: a cross-sectional study. BMC Womens Health. 2022;22(1):186.
Google Scholar
Hey HWD, Lim JXY, Ong JZ, Luo N. Epidemiology of neck pain and its impact on quality-of-life-a population-based, cross sectional study in Singapore. Spine. 2021;46(22):1572–80.
Google Scholar
Adams MA, Freeman BJ, Morrison HP, Nelson IW, Dolan P. Mechanical initiation of intervertebral disc degeneration. Spine. 2000;25(13):1625–36.
Google Scholar
Andreucci MA, Campbell P, Dunn KM. Are sleep problems a risk factor for the onset of musculoskeletal pain in children and adolescents? A Systematic Review. Sleep. 2017;40(7). https://doi.org/10.1093/sleep/zsx093.
Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Järvelin MR, Taanila AM, et al. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine J : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2010;19(4):641–9.
Google Scholar
Afolalu EF, Ramlee F, Tang NKY. Effects of sleep changes on pain-related health outcomes in the general population: a systematic review of longitudinal studies with exploratory meta-analysis. Sleep Med Rev. 2018;39:82–97.
Google Scholar