BBC
BBCChronic pain is a fact of life for many thousands of people in Scotland but a health board is trying to tackle the long-term use of highly-addictive drugs as a treatment.
NHS Fife has one of the highest prescribing rates in Scotland for medicines such as codeine and morphine but it is now taking steps to offer a wider range of treatments to help people with persistent pain become less reliant on medication.
Suzie Morley is one of the patients who has reduced her use of painkillers.
She first experienced shooting pains in her back 10 years ago.
It developed into chronic pain often leaving her unable to get out of bed or carry out domestic tasks. She says it affected friendships and her confidence.
“I’m never not in pain, it’s like my body is sitting screaming just now, but you live with it for so long that it becomes a part of you,” she says.
Pain management
Suzie still relies on some medication but has been working with physios and occupational therapists at Fife’s pain clinic in Dunfermline to find alternative ways to relieve symptoms.
“I have learned to use various tools,” she says. “Pacing is massively important for me.
“I use different types of meditation, different breathing skills to sooth my pain and relax my body.
“There are a lot of people who think medication should fix this, but at the end of the day, if you suffer like I do from chronic pain then you are never ever going to get fully relieved. “
Chronic or persistent pain is known to affect at least one in five adults in Scotland although the true figure may be more than a third (as high as 1.7 million people).
High-risk pain medicines (HRPM) including opioids and benzodiazepines are used to treat a range of chronic pain conditions.
Codeine, morphine, gabapentin and pregabalin are often used in the treatment of nerve pain while diazepam is used for muscle spasm.
Not only do these medicines come with a risk of side effects like drowsiness, constipation and nausea but longer-term use can lead to physical dependence with a greater risk of overdose.
The NHS says dependence and withdrawal are likely to be significant issues with these drugs while the Faculty of Pain Medicine estimates that between 8% and 10% of patients have been, or are, addicted to opioids prescribed for chronic pain.

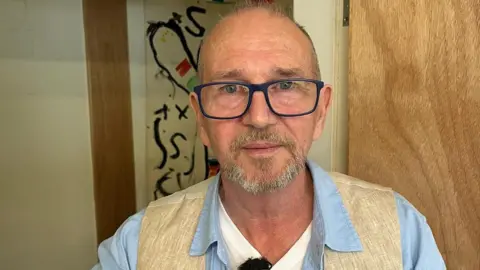
Deborah Steven is Fife’s lead pharmacist for pain management and the director of the high-risk pain medication programme.
She says that until recently clinicians saw powerful drugs as the best way to treat patients but a growing understanding that medicines are less effective for long-term pain is forcing a rethink.
“For short-term acute pain, medications are good, highly effective, really useful,” she says.
“For longer term chronic pain we definitely know they are not as effective.
“They benefit only about one in four people and they might only get a 30% reduction in pain.”
Ms Steven, who has researched chronic pain for more than 20 years, says getting rid of 100% of pain is not achievable and people will end up frustrated if that is what they expect medication to deliver.
“That then leads to patients going to see their healthcare professional for more support, possibly higher strengths of medicines or possibly asking for different medicines because something must help,” she says.
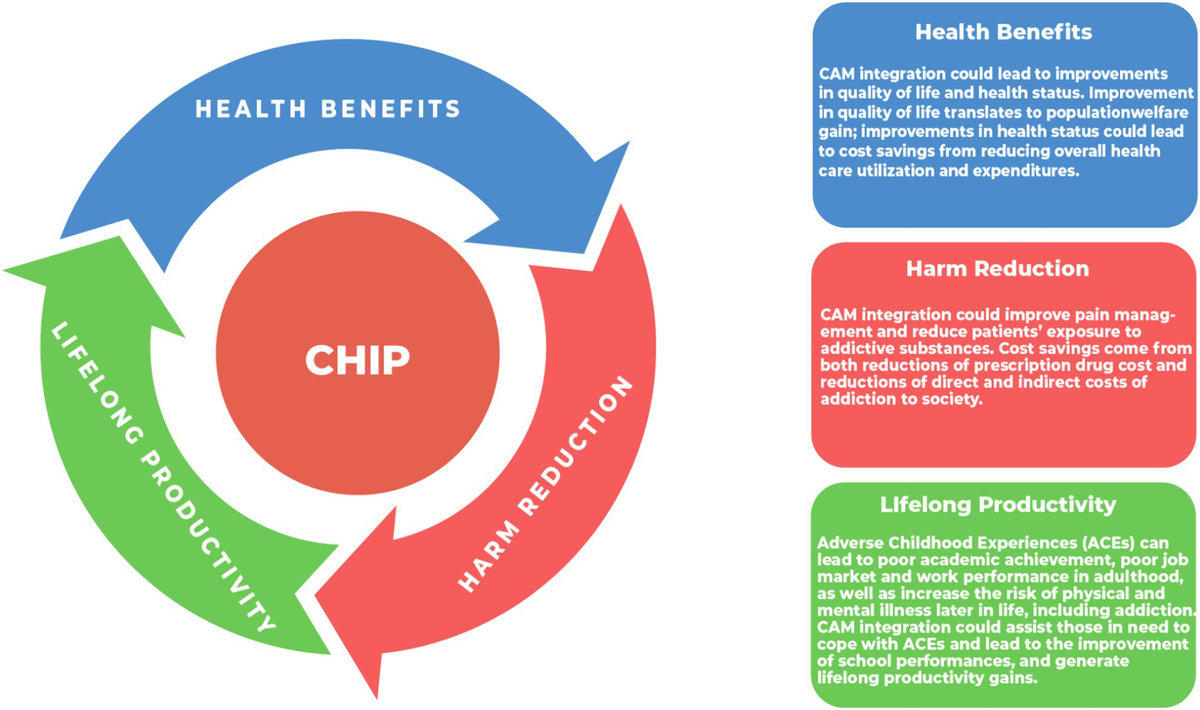
Instead of painkillers, her team is working with patients, GPs and clinicians to consider a wide range of interventions.
These includes physiotherapy, psychologists, occupational therapists as well as raising awareness that pain medications don’t solve everything.
There is also a dedicated Pain Talking website which has been developed as part of the programme.
Ms Steven says medicines definitely still have a place and patients should always consult with a healthcare professional before coming off prescribed drug.
But she says they are seeing positive results in Fife by offering alternative non-pharmaceutical treatments.
Charlie Marshall is another patient at the pain clinic.
He had a life-changing accident in 2013 when he was crushed by a car and has lived with fibromyalgia since.
Before his accident he was an industrial painter but after working with the clinic he now teaches art classes in Dalgety Bay as a way to take the focus off the pain he lives with.
“I had a sore head for six months,” Charlie says.
“There were times when I could hit my head off the bathroom wall.”
Charlie says he took a lot of medication including opiates and he felt like he had turned into a zombie.
Over a period of years, with the help of psychological support, he has reduced his use of painkillers and learned to live with some of his pain.
“My brain started to work a bit better,” he says.
“It was tough. It is a battle. You’ve got to want it and you can’t give in.”