The emergence of new PPS symptoms can result in functional decline in this population, which can be problematic when combined with previous sequelae. Muscle and joint pain are among the three most common symptoms in PPS that interfere with the performance of daily activities, as well as practical and occupational life, directly affecting quality of life16,17,18.
In the present study, all participants reported some level of pain, quantified as an average of 3 ± 0.79 on a 0–5 pain scale at baseline. However, in this study, pain was objectively measured using a standardized pain scale. Pain can become disabling if left untreated, negatively impacting the patient’s physical and mental well-being, and interfering with their daily activities and quality of life. As pain is influenced by cultural, emotional, and environmental factors, it has traditionally been seen as a subjective experience. Werhagen et al.19 evaluated the impact of pain on the quality of life of patients with PPS. The study found that patients who reported pain had worse quality of life in the SF-36 subdomains Body Pain (p < 0.001), General Health Status (p < 0.005), Vitality (p < 0.032), and for the Physical Compound Score (PCS) (p < 0.002) compared to those who did not report pain on clinical examination19.
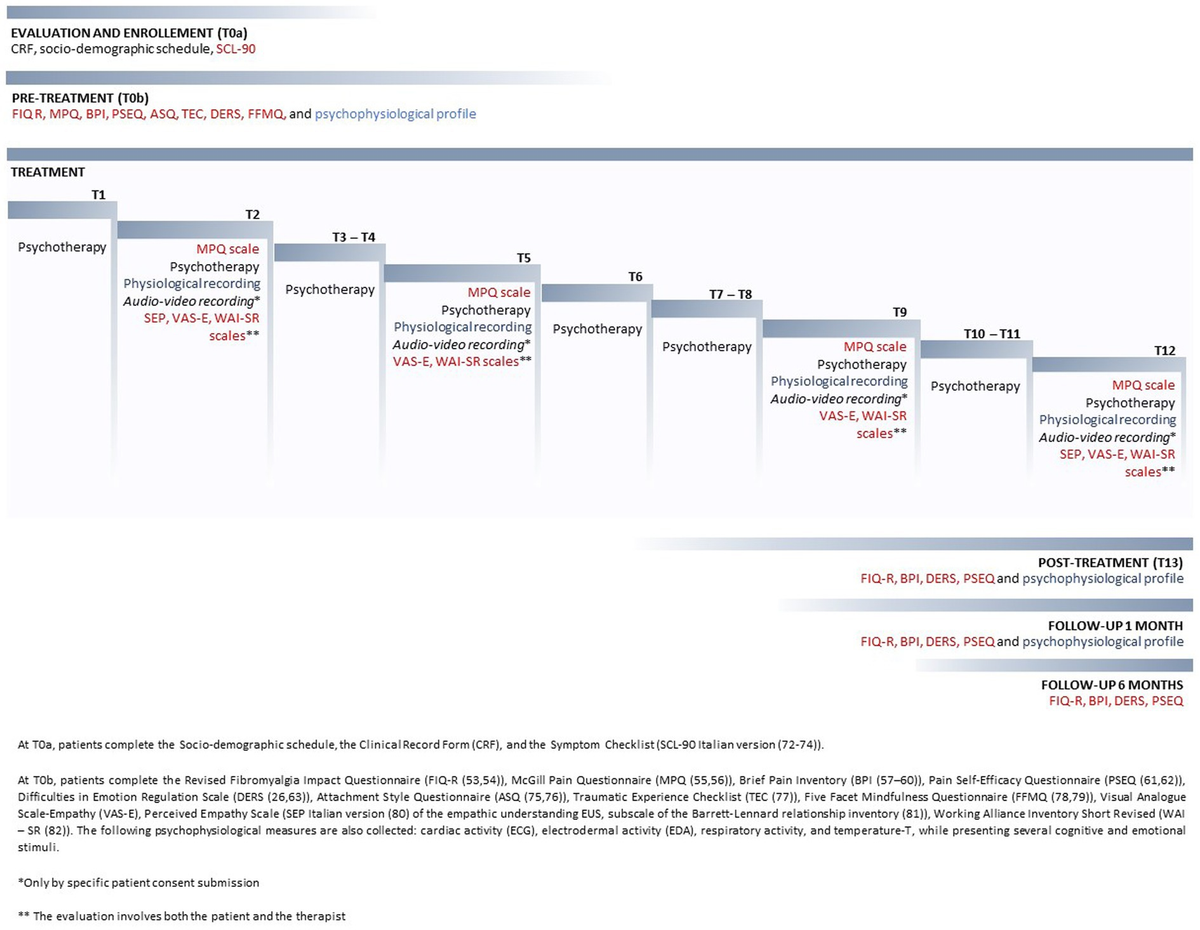
The present study utilized the McGill scale to assess symptoms in multiple domains, both quantitatively and qualitatively. The results indicate a statistically significant reduction in pain scores across all dimensions (sensory, affective, evaluative, and miscellaneous) following the application of the REAC protocols, compared to scores obtained prior to treatment (T0). Additionally, there were qualitative changes in pain perception, as evidenced by the reduction and variation of the McGill scale descriptors. In the sensory-discriminative dimension, which pertains to the mechanical, thermal, and spatial properties of pain20, the most common descriptors at T0 were ‘sharp’ and ‘pull’, which were replaced by ‘stinging’ at T4. The group associated with affective-motivational responses in individuals is linked to tension, anxiety, and neurovegetative responses20. The most frequent descriptor at T0 was ‘miserable’, while at T4 it was ‘disgusting’. ‘Problematic’ and ‘miserable’ were the most used words for the cognitive-evaluative component at T0, while at T4 it was ‘boring’. The miscellaneous dimension showed no change in the most frequent descriptor, which was ‘annoying’ at both T0 and T4. This presentation of descriptors is crucial for a qualitative assessment of pain and can assist in therapeutic intervention by providing a better definition20. These results indicate a broad impact of REAC protocols on participants’ pain perception.
Supporting these findings, a randomized, blinded, placebo-controlled study of 888 patients with clinically unexplained symptoms and presenting pain and physical problems showed a statistically significant reduction in both aspects after completing a cycle of NPPO21. Additionally, the intervention group exhibited a statistically significant reduction in the Psychological Stress Measure test score. According to the study, REAC technology is a non-drug and non-invasive alternative for treating pain, particularly in cases where emotional state and stress levels significantly impact overall symptoms21.
Regarding PPS, there has been much discussion about the physical aspects of the disease and the limitations it imposes on patients. It is worth noting that the emotional aspects of individuals diagnosed with post-polio syndrome can be influenced by their life history, as well as the clinical and social challenges faced during childhood. It is important to highlight that the care required for this condition can trigger children’s fears and suffering22. Shiri et al.5 found that emotional distress was higher in the polio sample than in the general population5.
The study assessed emotional state and stress levels using the DASS-21. Prior to treatment, 41.2% of participants reported experiencing some level of depression. The study was conducted during the COVID-19 pandemic, which may have negatively affected participants’ baseline mental health. Furthermore, 17.6% of the participants presented moderate depression at T0, a value that decreased to 0% at T4, demonstrating the benefits of the treatment. A study by Bryan J. Kemp23 evaluated 120 polio survivors and compared them with 60 healthy individuals, observing a 28% frequency of depression in the PPS group. Additionally, individuals with post-polio syndrome reported a higher average depression score in comparison to non-disabled controls and individuals with polio who either did not experience new symptoms or did experience new symptoms but did not meet the diagnostic criteria for PPS23.
Depression has a multifactorial origin. Depression scores have been negatively correlated with family function, health satisfaction, disability acceptance, Instrumental Activities of Daily Living (IADL) score, and PPS status for the sample of polio23. Jensen et al.24 found a correlation between depressive symptoms and increased pain and fatigue in individuals with post-polio syndrome24. Previous research has shown that individuals who experience a decline in their abilities and the onset of additional health problems, especially in clinical settings, may report more severe levels of distress. However, the extent of suffering and depression, as well as the impact of these changes on life satisfaction, are not yet fully understood23.
In this study depression, feelings of anxiety and stress were emphasized prior to the REAC therapeutic intervention. At T0, 64.7% of participants reported feeling anxious, with 23.5% reporting extreme anxiety. By T4, this percentage decreased to 6.3%. At the beginning of the study (T0), 76.5% of participants reported feeling stressed, with 29.4% reporting severe stress. By the end of treatment (T4), none of the participants reported severe stress. The study shows that the REAC therapeutic intervention effectively reduces anxiety and stress levels among participants. Additionally, a protocol involving 155 participants who reported mental and physical discomfort due to the Covid-19 pandemic showed a decrease in depression, anxiety, and stress scores after treatment with REAC NPPO-CB Neuromodulation, as measured by the DASS scale12. These results are of great importance, particularly given the impact of the COVID-19 pandemic, which has led to a rise in mental health issues in the general population.
PPS is a chronic and progressive condition that results in increasing limitations and challenges over time25,26. Dealing with the stress associated with these conditions affects an individual’s quality of life and overall well-being. Individuals with PPS face physical limitations related to their clinical condition, including movement, lifting, and transportation26,27. Garip et al.28 found that post-polio syndrome (PPS) negatively affects quality of life in terms of functional status, pain severity, and energy. Yang et al.27 reported that restrictions on mobility and activities have a greater impact on health-related quality of life in polio survivors than in the public, indicating that they have a particularly strong need for ongoing management and support27.
The study assessed quality of life using the WHOQoL-bref and found a statistically significant improvement in the physical and psychological dimensions between the T0–T3 and T0–T4 phases. These findings are consistent with Rinaldi et al.29 demonstration of the benefits of sequencing treatment protocols for people with Parkinson’s disease. The NPO protocol was applied, followed by the NPPO, resulting in an increase in functional capacity and improvements in the mental and physical health components of quality of life.
Research has shown that individuals who have survived polio experience limited mobility and activity, increased pain, and higher levels of depression and anxiety compared to both healthy individuals and the general population with activity limitations28. Additionally, sedentary behavior and insufficient physical activity can exacerbate several health problems, both physical and mental, which can directly impact the quality of life of those living with degenerative diseases. This research is significant in the treatment context, particularly considering the scarcity of therapies for this population.
The study demonstrated that REAC treatments had positive effects on pain control, anxiety, stress, depression, and quality of life in the patient group with PPS. Furthermore, it demonstrated an enhancement of the patients’ physical and mental health. No side effects were reported with the use of the REAC protocol in this research. Effective pain management is crucial for individuals with PPS, as pain is often related to depression, stress, and anxiety. The REAC neuromodulation protocols offer new insights that can help this patient population manage their pain and improve their overall health. Furthermore, REAC neuromodulation protocols show promise as a complementary intervention for individuals with active lifestyles, offering innovative ways to improve neuropsychological and physical performance in those with PPS. This has the potential to significantly improve overall quality of life.
Limitation section
REAC treatments may be an effective method for treating post-polio syndrome. However, further studies with larger sample and a study with a control group might provide more conclusive results.